Retinal detachment, symptoms, risks and treatment

Retinal detachment must be treated promptly. This is a dangerous alteration that absolutely should not be taken lightly. Focus on its factors, symptoms and treatments.
Retinal detachment: what causes?
The retina is the "thin layer that lines the back of the eye." Its different layers make it possible to receive and process the information sent to the brain via the optic nerve. Most often, during a detachment, a small pocket of intraocular fluid lifts the retina and prevents it from sticking, which causes visual loss on the detachment area. The detachment increases over time if it is not treated. This type of detachment is called rhegmatogenous retinal detachment .

There are also factors that facilitate retinal detachment. Among them:
- Age. From the age of 50, the vitreous body contracts and can lead to tearing of the retina
- Family history.
- The level of myopia.
- Eye operations.
- A detachment on the other eye (10% more chance)
- Eye trauma.
How do you know if you have retinal detachment?
It is not easy for a person to diagnose a detachment. However, the symptoms are explicit enough to force to consult an ophthalmologist. But they can be different depending on the degree of severity and the people. Thus, one can determine the presence of floating bodies , or the presence of a black veil on the periphery of the field of vision, the appearance of luminous points or flashes of light. All of these symptoms should not be taken lightly.
Of course, there is the possibility of having vision loss, partial or total, in the affected eye. This particular case requires urgent care.
What treatments and evolution?
The emergency consultation with the ophthalmologist takes place in three stages: a measurement of visual acuity, a measurement of ocular pressure and a fundus examination. Both eyes should be observed, even if only one is affected.
If detachment is determined, surgery will be required to apply the detached retina. In the majority of cases, the intervention takes place under local anesthesia, during outpatient surgery. Two techniques can be practiced. Medicare presents them as such:
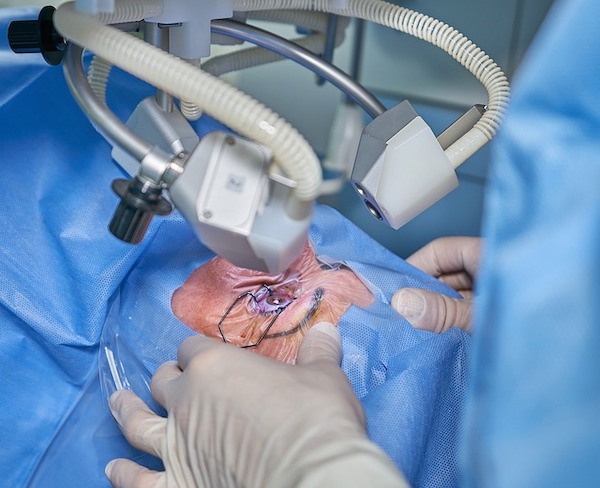
- Vitrectomy is the most common practice. It consists of removing the vitreous body responsible for the traction on the retina and obtaining the healing of the edges of the tear(s) by applying cold or laser. Gas or silicone oil are injected into the eye to hold the retina to the wall of the eye while it heals;
- cryo-indentation is performed without eye surgery. The tear(s) are closed by suturing a synthetic material to the outer wall of the eye. The subretinal fluid is punctured and the edges of the tear are healed by applying cold (cryo-application). In some cases, an injection of gas into the eye socket may be used to close the tear(s).
After surgery, rest is of course necessary. The surgeon will share certain contraindications in the days following the operation, due to the presence of eye gas. Thus, air travel and stays at high altitude will be prohibited until the presence of gas subsides.
If some customers complain of a few symptoms, it is therefore good advice to encourage them to perform a fundus examination. This examination can range from a simple precaution to a genuine means of anticipating a condition such as retinal detachment.
Sources: health insurance, cof.fr


